eStoreRx™
Online Supplement Dispensary
eStoreRx™ is an easy direct-to-patient ordering & fulfilment program for lifelong wellness.
For over 40 years, Biotics Research Corporation has revolutionized the nutritional supplement industry by utilizing “The Best of Science and Nature”. Combining nature’s principles with scientific ingenuity, our products magnify the nutritional
eStoreRx™ is an easy direct-to-patient ordering & fulfilment program for lifelong wellness.
Biotics Research is proud to expand our commitment to education with the Wellness Unfiltered Pro Podcast. Each episode delves into key health topics and the clinical applications of our premier products. Through candid, insightful conversations, our team offers practical guidance to keep you informed and empowered as a healthcare professional.
February 03 2026
From bodybuilders looking to bulk up to everyday folks trying to drop a few pounds, people have practiced tracking their food for decades. Tracking ca...
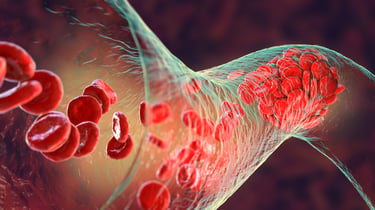 As the prevalence of metabolic syndrome, insulin resistance, and diabetes continues to grow, a recent publication sheds light on the temporal sequence of events that may contribute to their development and progression. Specifically, arterial stiffness has emerged as a possible precursor for subsequent events, including hyperinsulinemia and insulin resistance, at least in a younger population.
As the prevalence of metabolic syndrome, insulin resistance, and diabetes continues to grow, a recent publication sheds light on the temporal sequence of events that may contribute to their development and progression. Specifically, arterial stiffness has emerged as a possible precursor for subsequent events, including hyperinsulinemia and insulin resistance, at least in a younger population.
Published in the American Journal of Physiology: Heart and Circulatory Physiology, researchers from the UK and Finland continue to provide analyses of the associations between arterial stiffness and metabolic syndrome, in addition to cardiovascular risk factors, including hypertension, obesity, insulin resistance, and dyslipidemia, and perhaps most importantly, the suggestion that arterial stiffness may come first, and may be causative.
A series of papers have utilized data from the Avon Longitudinal Study of Parents and Children (ALSPAC) birth cohort, a subset of which (comprised of 3862 adolescents) was followed up for 7 years starting at age 17.7. All of the participants had multiple and repeated assessments, including dual-energy Xray absorptiometry (DEXA) to measure truncal adiposity, carotid-femoral pulse wave velocity (cfPWV) to determine arterial stiffness, carotid intima-media thickness (cIMT), and more typical measures of lipids and glucose, including homeostatic model assessment (HOMA) of insulin resistance and pancreatic beta-cell function.
A previous study from this cohort published in Hypertension found that higher cfPWV at age 17.7 years was associated with the risk of hyperinsulinemia by age 24.5. Additionally, increases of cfPWV and cIMT over the 7-year period were directly associated with increases in LDL-C and triglycerides, with modeling of this data indicating cfPWV came before the increases in insulin, as well as the worsening of insulin resistance and beta-cell function. Additionally, cfPWV worsening was directly associated with a 7-year increase in blood pressure, with an elevated cfPWV at age 17.7 associated with a 20-77% higher risk for both systolic and diastolic hypertension by age 24.5.
Obesity has also been linked to arterial stiffness in this population. Between the ages of 9 to 17, longitudinal adiposity measures (total and trunk fat mass index, (FMI)) were found to increase the risk of arterial stiffness by age 17. It’s important to note that adiposity was not defined by BMI in this study, and BMI along with waist-to-hip ratio would have misclassified at least 1/3 of these children, highlighting the importance of using FMI to correctly gauge risk. Between the age of 17.7 to 24.5, FMI was bidirectionally associated with arterial stiffness.
These findings in a younger cohort support previously published data in adults; in a study with nearly 9,000 participants in China (mean age 48), arterial stiffness (assessed by brachial-ankle pulse wave velocity (baPWV)) was associated with a 59-111% increase in risk for type 2 diabetes, and also appeared to precede increases in fasting blood sugar. Similarly, an older cohort (mean age ~72) in Sweden followed for 4.4 years found cfPWV to be a significant and independent risk factor for diabetes; compared to the lowest tertile of cfPWV, the 2nd and 3rd tertiles carrying an 83% and 224% higher risk, respectively, after adjustment for confounders. Arterial stiffness in adults is also clearly an independent risk factor for hypertension and may increase cardiovascular risk beyond its influence on blood pressure.
These associations are important not only because they may provide an early assessment of risk not currently captured, but also the temporal relationships suggest causality. This also implies that therapies which target arterial stiffness may offer additional benefit than only targeting the downstream effects. For example, metformin use in a younger population may not sufficiently protect against beta-cell deterioration, and in adults, metformin appears to have no effect on arterial stiffness, at least in people with type 2 diabetes, implying that all underlying causes are not being treated.
What is effective for preserving arterial elasticity? In adults, the Mediterranean diet may have some benefit. Data from a randomized trial (NU-AGE [New Dietary Strategies Addressing the Specific Needs of Elderly Population for Healthy Aging in Europe]) show that 1 year of adopting this diet significantly lowered systolic blood pressure and the augmentation index, a measure of systemic arterial stiffness, but unfortunately did not reduce arterial stiffness measured by cfPWV, considered the gold standard, and more reflective of stiffness in large arteries. Perhaps a longer study would have observed more of an improvement, but this has not been shown yet.
Exercise also appears to play a role, as does reducing truncal obesity. In a meta-analysis of 26 randomized and controlled trials that enrolled postmenopausal women, both aerobic and resistance exercise (particularly of low/moderate resistance intensity) were found to significantly reduce arterial stiffness, whereas data was not sufficient to find a similar benefit from mind-body exercises, such as Tai Chi and yoga. Data from the ALSPAC cohort suggests that in a younger population, cardiorespiratory fitness, lean mass, and fat mass all have bidirectional or temporal relationships with arterial stiffness, and improving cardiorespiratory fitness may be the appropriate focus of therapy. Arterial stiffness appears to be “a cause and a consequence of altered fat metabolism and deposit.” Encouragingly, although an elevated FMI was associated with arterial stiffness between the age of 9-17, reverting to a normal FMI over the study period was linked to normal measures of arterial stiffness, providing another target of therapy.
Submit this form and you'll receive our latest news and updates.
*These statements have not been evaluated by the Food and Drug Administration. This product has not intended to diagnose, treat, cure, or prevent any disease.
© 2025 Biotics Research Corporation - All Rights Reserved
Submit your comment